
When it comes to joint pain, most people think of medication or exercise — but what’s on your plate might matter just as much. Emerging research on Foods and Arthritis shows that diets high in sugar, refined carbs, and processed foods can quietly fuel inflammation, intensify stiffness, and slow recovery. These hidden triggers often go unnoticed in everyday eating habits, yet they can profoundly shape how your body feels and heals. In this article, we’ll explore how certain foods can worsen arthritis symptoms, and how mindful nutrition can help you reclaim comfort, energy, and control.
Why Diet Matters for Arthritis
Whether you’re dealing with Rheumatoid Arthritis (RA), Osteoarthritis (OA), or another form of joint condition, inflammation is a key player. Many forms of arthritis are driven or worsened by inflammatory processes in the body. Diet doesn’t cause arthritis on its own, but it can influence how strongly those processes behave.
Research has shown that certain foods, especially those high in refined sugars or heavy on processing, can push the body further into an inflamed state. In other words, your diet can either help turn the heat up on joint inflammation or help dial it down.
Refined Sugar: An Inflammation Booster
When we talk about “refined sugar”, we mean added sugars — the sweeteners, syrups and sugar-rich ingredients in processed foods, soft drinks, desserts, and even many convenience items. They aren’t just “empty calories”; they can have biological effects.
A key article from Verywell Health makes the point that sugar can cause inflammation in the body, which might make arthritis symptoms worse.
The piece goes on to say that you may notice worse arthritis symptoms if you eat a lot of added sugar.
Here are a few specific mechanisms and findings:
High intake of added sugar increases markers of inflammation in humans.
Among people with rheumatoid arthritis, studies found that desserts and sugar-sweetened soda were the most common foods reported to make symptoms worse.
For osteoarthritis, diets high in sugary foods and fat were associated with higher inflammation and worse joint breakdown. For gout (another form of inflammatory arthritis), high-fructose beverages raise uric acid levels, which is directly linked to gout flare-ups.
So at its core: added sugar = increased inflammation → which can mean the body’s joints and tissues are under more strain.
Processed Foods: More than Just Sugar
While sugar gets a lot of attention (rightly so), processed foods bring additional burdens that matter for arthritis:
Refined carbohydrates (think white bread, many snack foods) behave similarly to sugar in spiking blood glucose and triggering inflammatory responses.
Many processed foods contain high levels of trans fats, saturated fats, and an imbalance of omega-6 to omega-3 fatty acids, all of which influence inflammation.
Added sugars are hidden in surprising places: pasta sauces, yoghurts, cereals, bread, and canned soups. These “stealth” sugars contribute to the overall burden without us realising.
Processed convenience foods often displace healthier options (vegetables, legumes, whole grains) that help temper inflammation.
Therefore, when we talk about “processed foods”, we mean not just the sugary treats but the packaged, prepared meals and snacks that the modern diet leans on, and which may tip the balance toward more inflammation for a person with arthritis.
What It Means for You: Actionable Steps
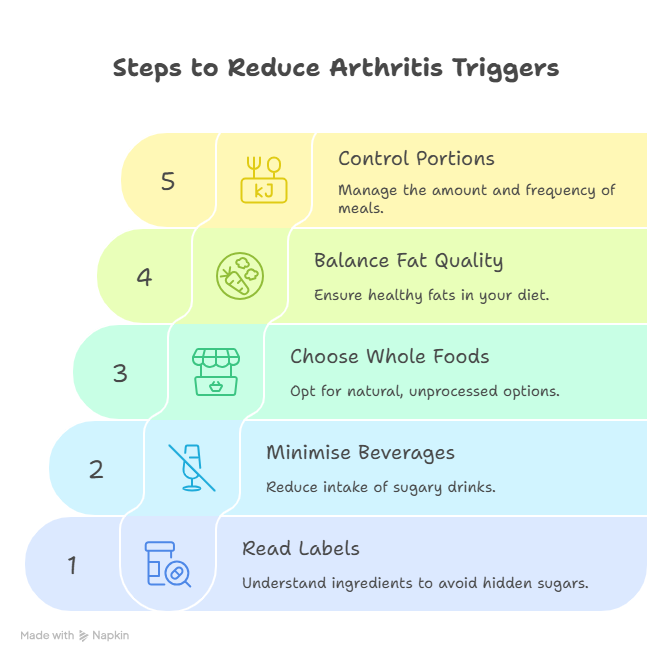
Here are practical, realistic steps you can take, informed by research and suitable for life in India (or elsewhere), to reduce dietary triggers of arthritis.
1. Read Labels & Spot Hidden Sugars
Check ingredients for cane sugar, corn syrup, fructose, high-fructose corn syrup, dextrose, maltose, evaporated cane juice, etc.
Also check nutrition facts for “added sugars”, aim to keep added sugar to less than 10% of daily calories, a guideline endorsed by the Centres for Disease Control and Prevention.
2. Minimise Sugar-Sweetened Beverages
In the Verywell article, sugar-sweetened sodas were strongly linked to increased arthritis risk and flare potential.
In India, that means considering soda, packaged fruit juices, sweetened tea/coffee, and even some energy drinks. Swap with water, unsweetened tea, or naturally-flavoured water.
3. Choose Whole Foods Over Processed
More vegetables, fruits, whole grains, legumes and less processed snacks and ready meals. For example, homemade chapatis, dals, and fresh vegetables instead of heavily processed biscuits, instant noodles, and fried packaged snacks.
Studies show that diets rich in plant-based, antioxidant-rich foods are associated with lower OA progression.
4. Balance Your Plate: Fat Quality Matters
It’s not just sugar, but also the fats in processed foods. Try to reduce saturated and trans fats, and include good fats from nuts, seeds, fatty fish (if you eat fish), or plant oils (prefer light uses of oils such as mustard, olive in moderation).
Also reducing processed meat, fried snacks, and packaged baked goods: typical of high-inflammation diets.
5. Keep Portion & Frequency in Check
Even healthy foods can contribute to inflammation if overeaten or if they lead to obesity, which is itself a risk factor for arthritis. The Verywell article points out that obesity and inflammation are tied, and they both hit joints hard. Verywell Health
Why This Matters — Especially for Arthritis Sufferers
Joint load + inflammation = worse outcomes. If your body is dealing with systemic inflammation (from diet, weight, etc), then your arthritic joints are under added pressure.
Immune system activation. In inflammatory types of arthritis (for example RA), heightened inflammation can accelerate joint damage. Dietary triggers may worsen this.
Quality of life. Less flare-ups, less joint swelling, less pain means more mobility, better function, and improved mood. Diet is one controllable piece of that equation.
Prevention mindset. Even if you don’t currently have severe arthritis, reducing high-sugar processed food intake can help delay joint issues, or reduce risk of developing more aggressive forms.
Summing It Up: Sugar + Processed Foods = Watch the Trigger
At PainPal.in, we believe in giving you actionable, practical insight. Here’s the short version:
High intake of added sugars and heavily processed foods can raise inflammation in the body.
For those living with arthritis, that means potential for worsened pain, swelling, and joint damage.
By choosing more whole, minimally-processed, low-added-sugar foods, you can help reduce the “background noise” of inflammation and give your joints a better chance to cope.
Always talk to your doctor or dietician before making big changes, especially if you have complex health conditions.
🩺 Final Thought
Sugar and processed foods may seem harmless, but for people living with arthritis, they can quietly amplify inflammation and worsen pain. The connection between diet and arthritis symptoms is well-researched and biologically plausible — refined sugars raise inflammatory markers, processed foods add trans fats and additives, and together they create an internal environment that stresses your joints.
The good news is that small, consistent dietary shifts can make a difference. Reducing added sugars, cooking more from scratch, and choosing fresh, nutrient-dense foods can help calm inflammation and support joint health.
At PainPal, we believe in empowering people with arthritis through awareness, science-backed information, and lifestyle strategies that truly help. Your plate has power; use it wisely, and your joints may thank you for years to come.
Frequently Asked Questions (FAQ)
1. Can sugar directly cause arthritis?
No. Sugar does not cause arthritis, but it can worsen inflammation and make symptoms more intense. Research shows that diets high in added sugar are associated with higher inflammatory markers, which may aggravate arthritis pain.
2. What foods are considered “processed” and should be limited?
Processed foods include items high in added sugars, unhealthy fats, preservatives, and refined carbs — such as packaged snacks, sweetened cereals, soda, fast food, processed meats, and baked goods like pastries and cookies.
3. How does inflammation relate to arthritis?
Inflammation is the body’s natural defence mechanism. In arthritis, chronic inflammation leads to joint swelling, stiffness, and pain. Foods that promote inflammation can make arthritis symptoms worse over time.
4. Are there any sweet alternatives that are safe for people with arthritis?
Yes. Natural sweeteners in moderation — such as small amounts of honey or jaggery — can be better choices than refined sugar. However, portion control still matters. Fruits are an excellent natural source of sweetness with added fibre and nutrients.
5. What are the best anti-inflammatory foods for arthritis?
Foods rich in omega-3 fatty acids (like flaxseeds, chia seeds, walnuts, and fatty fish), leafy greens, berries, turmeric, and olive oil have anti-inflammatory properties. Whole, plant-based diets can help reduce inflammation.


