
Arthritis—whether Rheumatoid arthritis (RA) or Osteoarthritis (OA)—is fundamentally characterised by inflammation in the joints. While medications, physical therapies and lifestyle adjustments are mainstays of management, an area of growing interest is how our diet helps modulate inflammation, and by extension how it may influence arthritis progression and outcomes.
In this post we explore the concept of anti-inflammatory dietary patterns (often characterised by a low dietary inflammatory index), what the research says about their link to arthritis (especially RA), and practical tips you can adopt. This is not a cure-all, but rather a piece of the puzzle for those looking at a holistic approach.
What do we mean by an “anti-inflammatory diet”?
An “anti-inflammatory diet” refers to eating patterns rich in foods that tend to reduce systemic inflammation (vegetables, fruits, whole grains, healthy fats, lean proteins) and limiting foods that may promote inflammation (refined carbs, excess saturated fat, processed foods, certain additives). As the Arthritis Foundation explains: “An anti-inflammatory eating plan emphasises whole foods, plants, healthy fats and lean protein, and limits processed foods, excess sugar, refined grains and saturated fat.”
Another way researchers measure this is the Dietary Inflammatory Index (DII): a scoring method that assigns a value to a diet’s inflammatory potential (higher = more pro-inflammatory; lower = more anti-inflammatory). For example, in the study from the journal Arthritis Research & Therapy, they used DII in combination with the Healthy Eating Index (HEI-2015) to assess diet and outcomes in RA. BioMed Central
So when we speak of a “low dietary inflammatory index diet,” we mean a pattern of eating that scores lower on the DII scale (i.e., less likely to provoke inflammation)
Why this matters for arthritis
Inflammation is the mechanism through which arthritis causes joint damage, pain and disability. If diet influences systemic inflammation, then logically it could influence arthritis onset, activity, progression and outcomes.
Here are some research highlights:
The Arthritis Research & Therapy paper found that among people with RA, those whose diets combined a high HEI-2015 (i.e., better overall diet quality) and a low DII (i.e., more anti-inflammatory) had a significantly lower risk of all-cause mortality compared to those on unhealthy + pro-inflammatory diets (hazard ratio ~0.70) after adjustment for confounders.
The same study noted that when looking at DII or HEI alone, the associations were not statistically significant—but the combination of healthy + anti-inflammatory mattered. Foundation page summarises that while individual foods or nutrients won’t “fix” arthritis, adopting a diet with more anti-inflammatory potential can support joint health and overall wellbeing.
Building a Low-Inflammatory Diet
A low-inflammatory diet is not a strict regimen but rather a pattern of eating that emphasizes whole, nutrient-dense foods rich in compounds that actively fight inflammation. The Mediterranean diet is the most recognized and well-researched example of this pattern.
To start reducing your body’s inflammatory response through diet, focus on these key anti-inflammatory food groups:
| Food Group | Key Anti-Inflammatory Components | Recommended Foods |
| Fatty Fish | Omega-3 Fatty Acids | Salmon, mackerel, sardines, tuna, herring. These healthy fats are powerful inflammation fighters. |
| Fruits & Vegetables | Antioxidants and Polyphenols | Berries (blueberries, strawberries), dark leafy greens (spinach, kale), broccoli, colorful peppers, and citrus fruits. Antioxidants neutralize the unstable molecules that cause cellular damage. |
| Healthy Fats | Monounsaturated Fats | Extra virgin olive oil (a staple in the Mediterranean diet), avocados, and nuts. |
| Whole Grains & Beans | Fiber | Whole-wheat flour, oatmeal, brown rice, quinoa, and various beans (kidney, pinto). Fiber helps lower the inflammatory marker C-reactive protein (CRP). |
What the evidence shows (and its limits)
What we can say:
There’s credible evidence that diets with lower inflammatory potential (i.e., lower DII) are associated with better outcomes (in this case, survival) in people with RA.
Healthy eating patterns (vegetables, fruits, fish, whole grains, plant proteins, limited saturated fat) are widely recommended for general health, and are likely beneficial for people with arthritis too. Dietary advice emphasising anti-inflammatory foods is safe and sensible as part of a broader management plan.
What we cannot claim (yet):
That eating a low-DII diet will definitively slow joint damage or reverse arthritis. The mortality-study was observational (so cannot prove causation) and focused on RA, not necessarily OA.
That one specific diet is best for everyone with arthritis—individual responses vary (age, sex, body weight, comorbidities, type of arthritis).
That diet alone replaces medications, physical therapy, exercise or medical supervision. Diet is a complementary strategy, not a standalone cure.
In short: adopt diet changes as part of your arthritis-management toolkit, but continue working with your doctor, physiotherapist or rheumatologist.
Tips for someone with arthritis
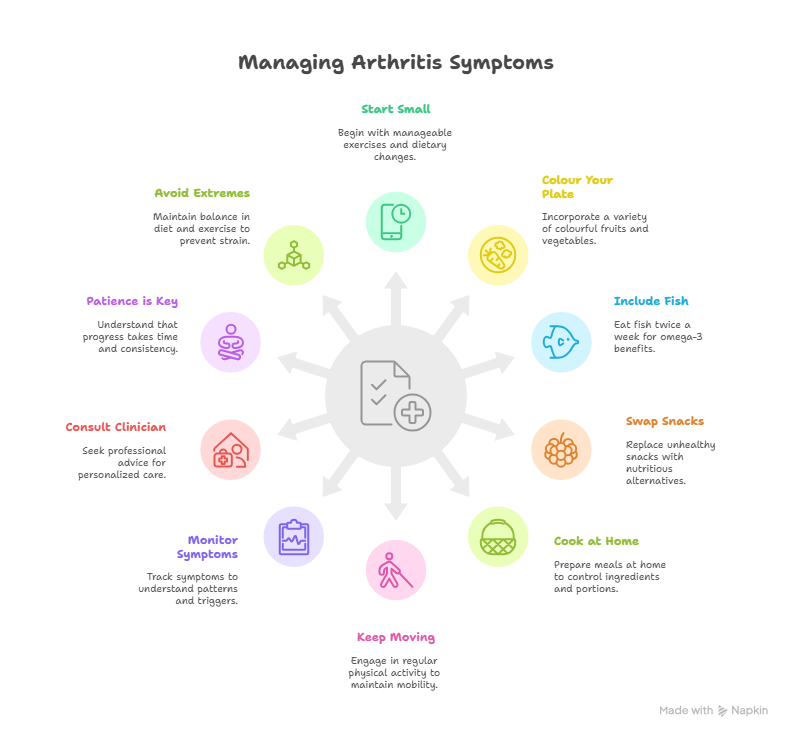
Guidance on arthritis and lifestyle, here are some actionable tips:
Start small: Pick one meal and “upgrade” it. For example, instead of white rice, try a whole-grain alternative once a week.
Colour your plate: Make sure half your plate is vegetables/fruits. The more colours, the better the variety of phytonutrients (potentially anti-inflammatory).
Include fish twice a week: It provides omega-3, which has anti-inflammatory effects.
Swap snacks: Substitute sugary biscuits with nuts + fruit or seeds.
Cook more at home: Enables you to control ingredients (oil, salt, sugar) and reduce processed food reliance.
Keep moving: Diet alone won’t do it — gentle activity, joint-friendly exercise, and weight management boost the benefits.
Monitor your symptoms: Note how diet changes make you feel (pain levels, stiffness, energy). Over time, you may notice a pattern.
Consult your clinician: If you have comorbidities (diabetes, heart disease, kidney issues), tailor diet with professional support—some anti-inflammatory foods might need modifications in special cases.
Patience is key: Changes take time to show effects; also, research shows that associations with like-minded people help in maintaining good health. (not guarantees).
Avoid extremes: Highly restrictive diets can sometimes lead to nutrient deficiencies. Aim for balanced, sustainable eating patterns rather than “quick fixes”.
Final thoughts on Anti-Inflammatory Diets
f you’re living with arthritis, you do have the capacity to influence your disease journey via what you eat — not in isolation, but as part of a holistic approach. Research (for example, the recent NHANES-RA study) shows that better diet quality and lower dietary inflammation are associated with improved survival in RA.
That said, diet isn’t a miracle cure. It’s a supportive tool. By adopting a dietary pattern with a lower inflammatory potential (i.e., a low DII) and higher overall quality — such as Anti-Inflammatory diets rich in whole foods, omega-3s, and antioxidants — you may help reduce systemic inflammation, support joint health, and enhance your overall well-being.
For many, experimenting with Anti-Inflammatory diets can also serve as a gateway to more mindful eating — one that nourishes not just the joints, but energy, sleep, and mood.
As always, discuss diet changes with your healthcare provider, especially if you are on medications or have other health conditions. And remember: each person’s journey is unique — what matters most is consistency, moderation, and supporting your body with good nourishment over time.
FAQs: Anti-Inflammatory Diet and Arthritis
1. Can an anti-inflammatory diet cure arthritis?
No, an anti-inflammatory diet cannot cure arthritis, but it can help manage inflammation, reduce symptoms like pain and stiffness, and improve overall wellbeing. It’s a complementary strategy that works best alongside medication, physiotherapy, and other medical care.
Source:
2. Which foods are proven to fight inflammation in arthritis?
Research suggests that foods rich in omega-3 fatty acids (like salmon, sardines, walnuts, flaxseeds), fruits and vegetables (especially leafy greens and berries), and whole grains may lower inflammation. Spices such as turmeric and ginger can also play a supporting role.
3. What is the Dietary Inflammatory Index (DII) and how does it relate to arthritis?
The Dietary Inflammatory Index (DII) measures how inflammatory your overall diet is—higher DII scores mean a more pro-inflammatory diet, while lower scores mean a more anti-inflammatory one. A recent study in Arthritis Research & Therapy (2024) found that people with rheumatoid arthritis who followed a low-DII, high-quality diet had lower all-cause mortality.
4. Are there specific diets recommended for people with arthritis?
While no single diet fits everyone, researchers often point to patterns like the Mediterranean diet or plant-forward diets as beneficial. These diets naturally align with a low DII, meaning they contain more anti-inflammatory foods and fewer processed items.
5. How long does it take to see results from dietary changes?
Every person is different, but most people notice subtle improvements in energy and inflammation markers within a few weeks to a few months of consistent changes. However, for joint pain relief and functional improvement, results may take longer and depend on the type of arthritis and other treatments used.


